5 Steps to Expect COBRA Paperwork Arrival Time

Step 1: Employment Termination Notice

When an employee experiences termination or resigns from their job, the first step in the COBRA (Consolidated Omnibus Budget Reconciliation Act) paperwork process involves receiving the official termination notice from your employer. This document is critical because it initiates the timeline for when you should expect to receive your COBRA election notice:
- Your employer is legally obligated to notify the plan administrator within 30 days after your employment ends.
- This notice to the plan administrator must include your name, last known address, and the date your employment ended.

📅 Note: The employer's responsibility to notify the plan administrator is crucial, as it sets the stage for the subsequent steps in COBRA continuity of coverage.
Step 2: Plan Administrator Notification

Following the notification from your former employer, the plan administrator has a legal timeframe within which they must send you the COBRA election notice:
- The administrator must send you the notice within 14 days after they've been notified by your employer.
- This means you can expect to receive your COBRA paperwork approximately 44 days after your employment terminates.

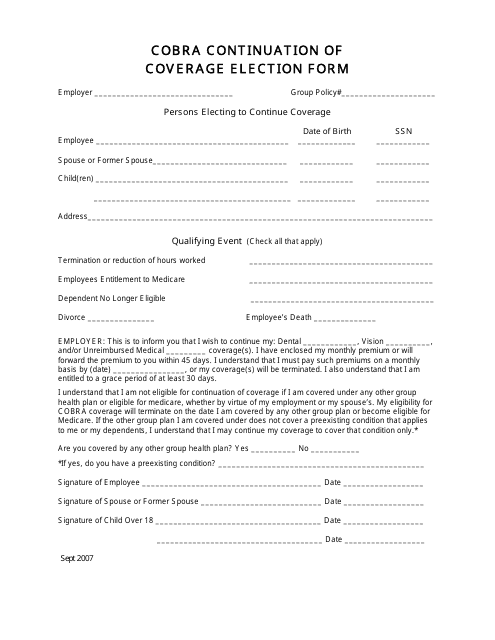
Step 3: Election Notice Delivery

Upon receiving the COBRA election notice, you must make some important decisions:
- Read through the notice carefully as it outlines your rights to continue health coverage.
- You'll typically have 60 days from the later of the date you lose coverage or the date you receive the election notice to decide if you want to elect COBRA continuation coverage.
| Event | Days |
|---|---|
| Employment Termination | 0 |
| Employer Notifies Plan Administrator | 30 |
| Plan Administrator Sends Election Notice | 44 |
| Your Election Deadline | 60 (after receiving the notice) |

Step 4: Payment of Premium

If you elect to continue your health coverage through COBRA, the next step involves understanding and arranging for premium payments:
- You have 45 days from the date you elect COBRA to make your first premium payment.
- This payment will retroactively cover the period back to the date your group health plan coverage ended.
- The premiums will be 102% of the plan's cost, accounting for administration fees.
💳 Note: Ensure you have your financial resources ready as COBRA premiums can be significantly higher than your former employer contributions.
Step 5: Continuation of Coverage

Once all paperwork is completed and payments are arranged, your COBRA coverage becomes effective:
- This coverage can extend for up to 18 months in case of job loss, or up to 36 months in other qualifying events like divorce or death of the covered employee.
- Make sure you receive confirmation of your coverage from the plan administrator.
In essence, following these steps closely ensures that you do not experience a gap in your health insurance:
- Know the exact date your employment ends.
- Stay updated with your former employer's timeline in notifying the plan administrator.
- Understand the COBRA election notice and act within the given timeframe.
- Arrange for premium payments in a timely manner.
- Enjoy the continuity of your health coverage under COBRA.
By staying proactive and well-informed about the timing of these events, you can transition smoothly to COBRA coverage, maintaining your access to necessary health services without interruption. Remember that COBRA provides an invaluable lifeline of health insurance for those experiencing changes in employment status, offering peace of mind during uncertain times.
What happens if I miss the COBRA election deadline?

+
If you miss the election deadline, you will generally lose your opportunity to elect COBRA continuation coverage. However, in some cases, special considerations might apply, such as extenuating circumstances or errors by the plan administrator.
Can I change my mind after I elect COBRA?

+
Yes, you can change your mind after electing COBRA, but you must notify the plan administrator. Once you’ve decided to revoke COBRA, coverage will end from the date you notify the plan, and no further premiums will be due.
What if I don’t receive the COBRA paperwork?
+
If you don’t receive the COBRA paperwork within 44 days from your termination date, contact your former employer’s human resources or the plan administrator immediately. There might have been an oversight or issue with the address on file.
Is there an age limit for COBRA?

+
There is no age limit for electing COBRA, but for certain qualifying events like reaching the age of majority, dependent children might lose eligibility. Check your plan specifics for details.



