5 Key Times to Send COBRA Paperwork
COBRA paperwork is crucial for employers and former employees alike. Understanding when to send this paperwork can ensure that employees continue to have access to healthcare coverage post-employment, preventing lapses that could result in medical expenses without insurance. Let's delve into five key times when it's critical to send COBRA paperwork.
1. Upon Termination of Employment
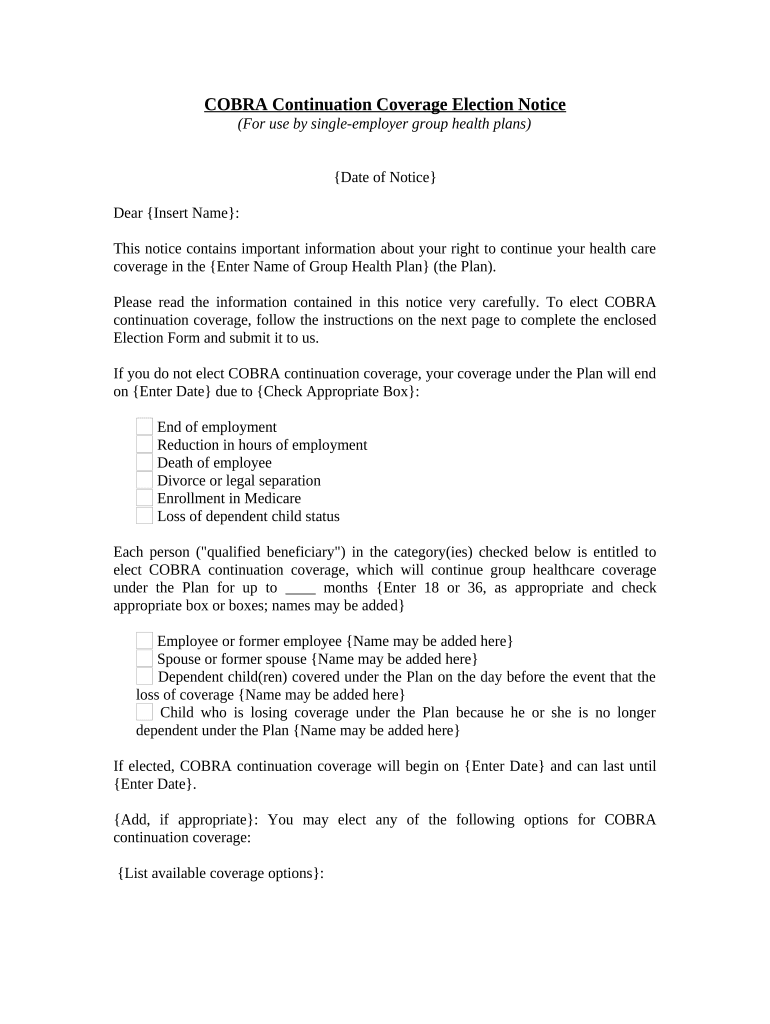
One of the most common triggers for sending COBRA paperwork is when an employee's employment ends. Here's what employers need to do:
- Notify the employee: Send COBRA paperwork within 44 days of the termination.
- Ensure the employee understands: Provide clear information about their rights to continue health coverage.
2. Reduction in Work Hours

A reduction in work hours that causes an employee to lose eligibility for the company's group health plan is another pivotal moment:
- Send COBRA paperwork promptly to avoid any coverage gaps.
- Explain the situation and potential health coverage implications.

3. During Leaves of Absence

Employees who take extended leaves of absence, whether for medical reasons or family matters, might also need COBRA paperwork:
- Send COBRA information when there is uncertainty about the employee's return or a risk of losing health benefits.
- Ensure the documentation includes details about how leave affects their insurance.
🚨 Note: Employees might not realize that their leave could affect their health coverage. Clear communication can prevent misunderstandings.
4. On or Before Retirement

Retirement is a significant life transition where COBRA paperwork becomes relevant:
- Provide COBRA details as part of the retirement package.
- Highlight the option for continued health coverage until they qualify for Medicare.
5. Post-Divorce or Death of an Employee

In situations like divorce or the death of an employee, sending COBRA paperwork timely is not just helpful but legally necessary:
- In case of divorce, ensure the employee's spouse or former spouse receives COBRA information within 30 days.
- If an employee dies, their family members or dependents need to receive COBRA paperwork promptly to maintain their health coverage.
| Event | Timeframe for Sending COBRA Paperwork |
|---|---|
| Termination of Employment | Within 44 Days |
| Reduction in Work Hours | Promptly |
| Leaves of Absence | When Coverage is at Risk |
| Retirement | As Part of Retirement Package |
| Divorce/Death | Within 30 Days |

In sum, timely distribution of COBRA paperwork during these critical junctures not only complies with legal requirements but also demonstrates your organization's commitment to the health and well-being of its employees. From termination to leaves, retirements, and family transitions, being proactive in sending COBRA documentation ensures continuity of care, which is essential for your former employees' peace of mind.
What happens if COBRA paperwork is not sent on time?

+
If COBRA paperwork is not sent within the required timeframe, you could face penalties, and employees might lose their right to elect COBRA continuation coverage.
Can former employees receive COBRA if they move out of state?

+
Yes, COBRA coverage can continue even if an employee moves out of state. However, they should check if their current healthcare providers are in the network or consider switching plans if necessary.
Is there a deadline for employees to elect COBRA coverage?

+
Employees have 60 days to elect COBRA from the date of notification or the date of the qualifying event, whichever is later.