Get Your COBRA Paperwork Fast: Insider Tips

When you're facing a life event that separates you from your employer's health insurance, like job loss, divorce, or transitioning between jobs, the Consolidated Omnibus Budget Reconciliation Act (COBRA) provides a crucial safety net. COBRA allows you to continue your group health plan coverage for a limited time, but navigating through its paperwork can often feel daunting. Here’s how you can expedite the process and ensure you don't miss out on this essential benefit.
Understanding COBRA Eligibility and Deadlines
Before you dive into the paperwork, it’s vital to understand when you’re eligible for COBRA continuation coverage:
- You must have been covered by your employer’s group health plan at the time of the qualifying event.
- The employer must have had at least 20 employees on more than 50% of its typical business days in the previous calendar year.
Additionally, you should be aware of these key deadlines:
- You have 60 days from the later of the date you receive the COBRA election notice or the date of the qualifying event to elect COBRA.
- After electing COBRA, you have 45 days to make your first premium payment.
Don't let these dates slip through your fingers; timely action is critical for seamless coverage continuation.
Steps to Obtain COBRA Paperwork Quickly

Here’s a step-by-step guide to get your COBRA paperwork efficiently:
-
Notify Your Employer
If you’re still employed when your qualifying event occurs, notify your employer immediately. This can be a change in employment status, reduction in hours, or other events that qualify you for COBRA.
-
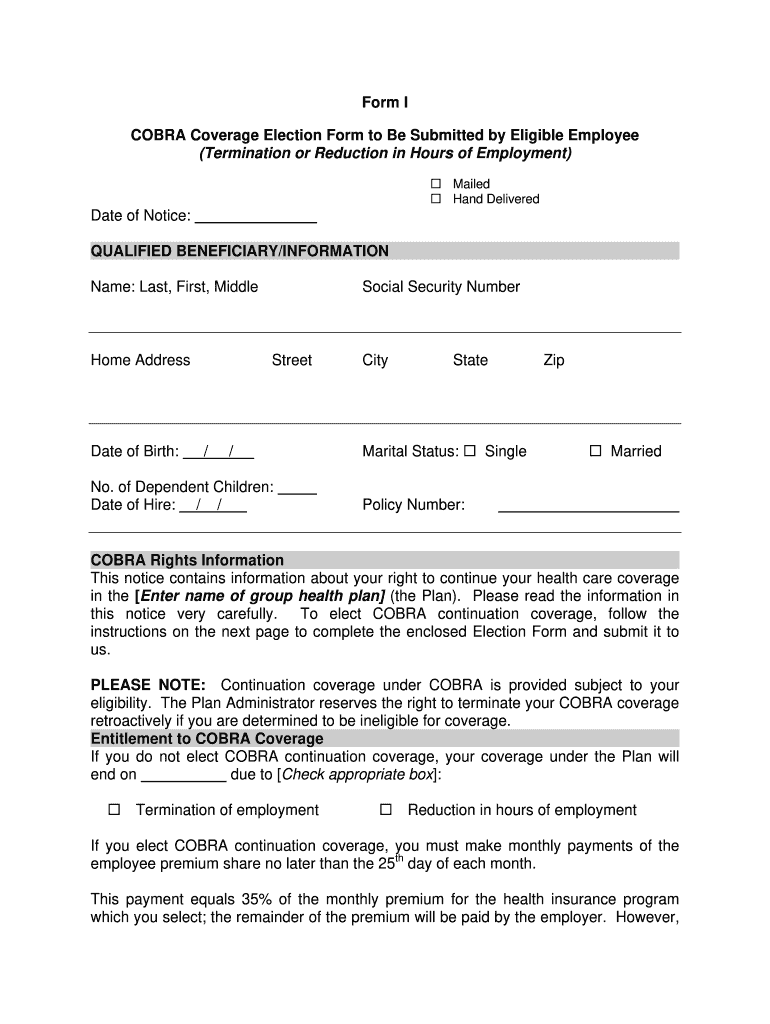
Request COBRA Notice and Enrollment Packet
Ask your HR department for the COBRA election notice, which includes all the necessary paperwork to enroll in COBRA.
-
Check for Online Resources
Many companies now provide online portals or direct links to download COBRA forms. Ensure you look on your employer’s internal HR site or their official employee benefits portal.
-
Make Contact with COBRA Administrator
If your company uses an external COBRA administrator, their contact information should be on the initial notification of your qualifying event. Reach out to them for any missing documentation.
-
Fill Out Forms Carefully
Complete the forms with accurate information, double-checking all personal details, and ensuring your payment options are clearly indicated.
⚠️ Note: Make sure to keep copies of all documents you send for your records.
Common Issues and How to Overcome Them
While the process seems straightforward, issues can arise:
- Delayed Notifications: Sometimes, employers might delay notifying you about COBRA, which can shrink your enrollment window. Keep in touch with HR or the COBRA administrator if you anticipate delays.
- Confusing Paperwork: If the forms or notices seem confusing, don’t hesitate to contact the HR department or COBRA administrator for clarification.
- Payment Issues: Be proactive about understanding the payment process. Issues with mailing checks or setting up electronic payments can delay your coverage.
Streamlining COBRA Enrollment

To make your COBRA enrollment as smooth as possible:
- Stay Organized: Keep a file with all relevant documents, communications, and deadlines.
- Set Reminders: Use digital reminders for key dates like when you must elect COBRA, when your first payment is due, and when future premiums are due.
- Ask for Help: Utilize resources like healthcare.gov for guidance or legal aid if you feel you’re being treated unfairly or if there are complications.
By being proactive and using these tools, you can streamline the COBRA enrollment process, ensuring continuous health coverage when you need it most.
Understanding and swiftly navigating COBRA paperwork is critical to ensure you don't face a gap in healthcare coverage. This safety net not only provides you with peace of mind but also prevents any unexpected medical expenses. If you follow these insider tips, you'll be well-equipped to manage your COBRA enrollment efficiently, securing your access to health care when it matters.
What events qualify for COBRA continuation?
+
Events like termination of employment, reduction in hours, divorce, death of the covered employee, or becoming eligible for Medicare can qualify someone for COBRA continuation.
Can COBRA be extended beyond the standard period?
+
Yes, under certain conditions like a second qualifying event, the initial 18-month coverage can be extended up to 36 months.
How does COBRA work if I already have other insurance?

+
Even if you have other insurance, COBRA can act as secondary coverage, helping to cover costs that your primary insurance might not.